How to Interpret Your Bone Density Scan Results
How to interpret your bone density scan results
So, your GP has had you get a scan to assess your bone density. You might even have a copy of this scan and a brief explanation of what it means, but let’s be honest – sometimes the numbers can be a little confusing. Let’s take this a step further and work out what your results really mean!
Your bone density is measured via a DEXA scan, which stands for Dual-Energy X-Ray Absorptiometry. This is a non-invasive exam that utilises low dose x-rays at two different energies to distinguish between bone and soft tissue. This test can also measure your body composition, such as body fat and muscle mass, but primarily is utilised as the gold standard in diagnosis for risk of osteoporosis and fractures. The exam is usually performed at the most common fracture sites: the spine, hip or wrist. I believe it is important for all women over the age of 50, and men over the age of 60, to have a DEXA scan so that you have a baseline for your bone density that can be monitored as you are getting older. This is also the same if you have any risk factors including family history, early menopause, hormonal treatments such as a lot of cancer medications, or conditions such as coeliac disease that affect your calcium absorption. If this sounds like you, have a chat to your GP about checking your bone density. Osteoporosis is common, affecting around two out of every three women, and one in six men, over the age of 60. Osteopenia is when your bone density is low, however not low enough to be classified as osteoporosis, with nearly two-thirds of Australian’s over 50 affected.
But let’s delve into what your DEXA results are telling you…
The locations
These are some of the locations that your DEXA scan might show:
AP spine L1-L4: This is a snapshot of the entire segment of your lower back (or lumbar spine). You might also see L1/L2/L3/L4 with their own row, which looks specifically at those vertebrae.
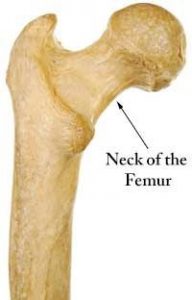
Femoral neck: Despite what the name might suggest, this is actually not in your neck but in your hip. As you will see below, this is the narrow part of your femur that lies just underneath the head of the femur (which forms our ball and socket joint). The reason this particular location is assessed because it is strong predictor of hip fracture susceptibility.
Total hip: This looks at the entire hip region (including the femoral neck).
Wrist: Sometimes the wrist is utilised as a site if access to the spine or hip is restricted (e.g. had a hip replacement or other metal structures in the spine).
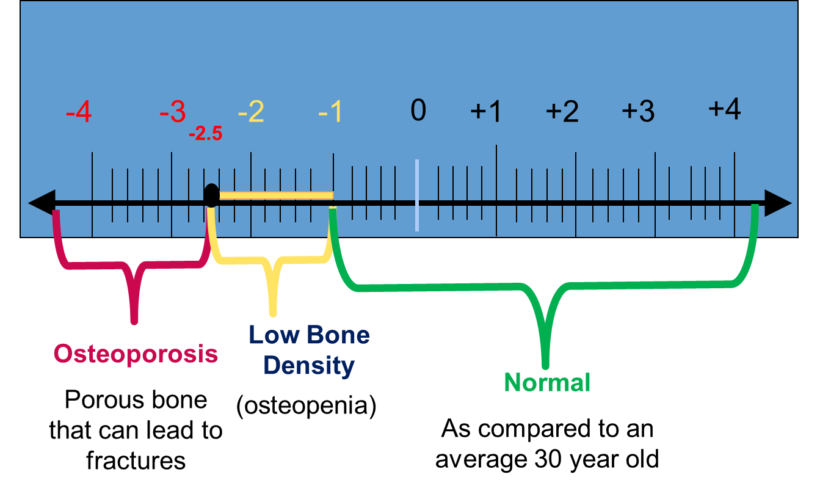
T-Score
The T-score indicates how your bone density compares to that of a healthy 30 year old. The reason for this is because peak bone density is reached by age 30 and should ideally be maintained at this level throughout your life. The T score shows whether your bones are more dense (+) or less dense (-) than those of an average 30 year old. This is the most important value and the one that is used to classify as normal, osteopenia or osteoporosis.
T-score 0 to –1 is considered normal.
T-score –1 to –2.5 is considered osteopenia.
T-score –2.5 is classified as osteoporosis.
The lower your T-score is below –2.5, the greater your risk of fracture.
Z-Score
This compares your bone density to that of an age-matched person. There are no specific categories for our Z score and it is not used in the diagnosis of osteoporosis, however it can give you a bit of an indication as to whether your bone density is common for someone of your age. The closer this number is to zero, the closer it is to what we might expect for someone of your age. If this number is above zero (+), you have more bone than this baseline, and if the number is below zero (-), it is below this baseline.
So I now know my classification, what does this mean for me?
Firstly I think it is incredibly important to have this education and understanding so that you can make informed, proactive decisions about your bone health. Being told you have osteopenia or osteoporosis is one thing, but when you can truly understand your risk it allows you to be involved in the management of your condition. Exercise is one of the most effective strategies to manage bone health and prevent further loss in bone, however not all exercise is equal when it comes to bones. So, if you have been diagnosed with osteopenia or osteoporosis, please ensure to book in with our Accredited Exercise Physiologists to have a chat about how we can support you. We can also help you interpret your bone density scans!
Tamika Hassum
Accredited Exercise Physiologist
